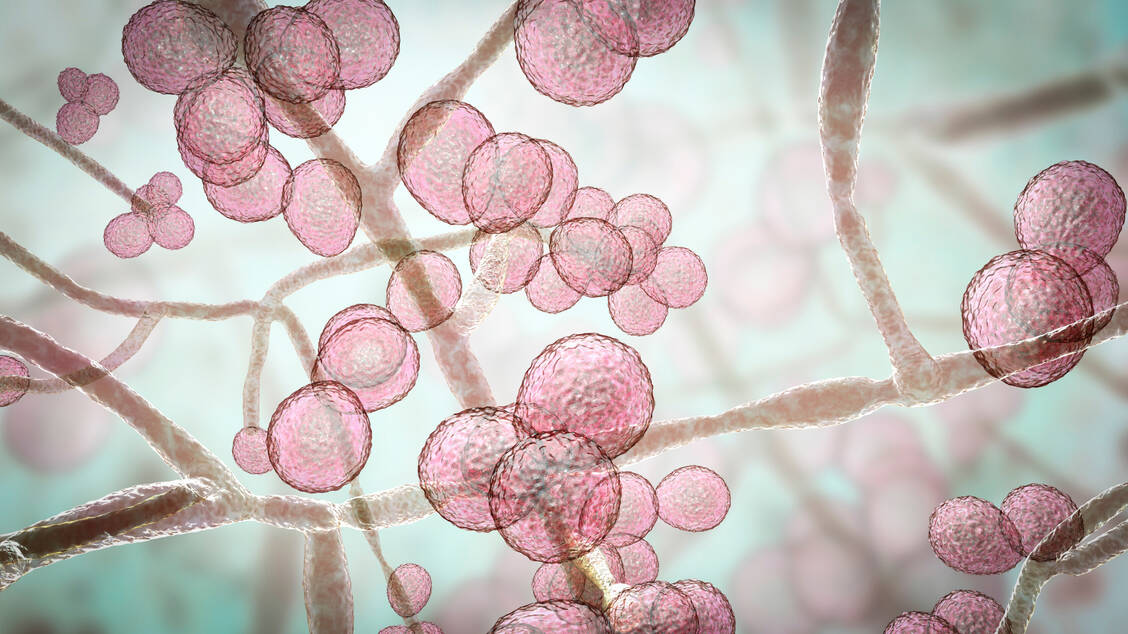
Candida auris colonises the skin and mucous membranes, including the ears, hands, nose, armpits, groin, throat and wounds as well as the intestines, respiratory tract and urinary tract. Infection poses a particular risk to immunocompromised patients, those with serious preexisting conditions or chronic illnesses. Even if the number of cases has so far been limited, experts consider the spread to be worrying. This is because if the fungus enters the bloodstream, the infection is fatal in 30 to 60 per cent of cases. Only a few antimycotics are available for treatment. The resistance rate to fluconazole is already over 80 per cent. Also, the infection often no longer responds to the echinocandins drug class. Such multiresistance, which is common in bacteria, is rather unusual in fungi. Experts therefore advise increased vigilance, but also emphasise that the fungus poses no danger to healthy people.